Interviewsand Articles
Interview with James Seeba: Medicine Journey
by Richard Whittaker, Apr 2, 2001
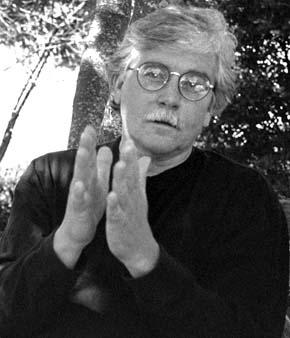
James Seeba was an early visitor to China after its reopening to the West where he studied the traditional Chinese healing arts of herbal medicine and acupuncture. In addition, Seeba is a careful follower both of new developments in alternative medicine and current medical research. He practices in Santa Rosa California.*
As we begin recording, Seeba is talking about his experiences in China. His wife Arly sits nearby....
James Seeba: When we were practicing in the hospital, or were in the class room, there would be this "shadow government" following along—a member of the Communist Party. Of course all the doctors and professors were careful about what they said. If this "shadow" would happen to be absent for a while, the difference in demeanor was remarkable. Remember, this was the time immediately following the collapse of "the Cultural Revolution" with its barbaric treatment of doctors and professors. Well, there was this fellow assigned to watch us named "De Long"— a very arrogant and demeaning character. "De Long" pronounced with one set of accents means "dragon," which was much to his liking. But if you change the accent a little it becomes "earthworm." And so, being the irreverent Americans that we were with our sympathies aligned with our professors, we would greet Mr. De Long each morning with great reverence, "Good morning Mr. Earthworm." You could see him just ready to burst and the professors knew exactly what was going on. Underneath their neutral faces their eyes would just be twinkling.
Richard Whittaker: (laughs)… But, I’m still thinking about something you were talking about earlier: the idea that something could be passed along through the body. Or, at least, that the body is the carrier of something fundamental which goes beyond politics, ideas, and so on. You described this impression that came from your experience of being among the Chinese people.
Seeba: It was astounding to us. I talked to my wife about it and she felt it too, this sense of something being very different. You couldn’t quite put your finger on it. While visiting Shanghai—one of those cities where there are so many people they stagger their days off, because if they all had Sunday off the city would be paralyzed…
Arly Seeba: Their streets are like freeways of people. Just masses of people…
Seeba: And the mass would open up and let a bus come through and then close up behind it again.
Arly Seeba: If you wanted to go into a store you had to start one or two blocks early, and start shifting to the right or to the left. Sometimes you’d get carried past by the crowd and would have to turn around somehow and go back. And yet amongst all that, they never seemed to touch each other. In all that time we were never bumped or jostled-just these thousands of bodies passing by ever so closely. It was a wonderful impression. It was like this consideration, not a mental one, but a physical consideration for your presence.
Seeba: They seem to be in their bodies in a certain way, and being in the midst of them—all passing each other freely—being in the midst of that created the strangest impression.
RW: And, as Americans, out of your own context, you must have been able to see something about yourselves…
Seeba: It became obvious, in relief, not only that I held a kind of tension—but that I lived in this tension. It was interesting to come out of our hotel each morning, for instance, and see everyone in the streets and the courtyards doing Tai-Chi. They were beginning their days doing movements that require a certain amount of attention and a certain amount of relaxation in order to assume the right form. This is not to romanticize the situation or ignore the distortions that exist in that society—but there is something which is observable in the quality of the movement. I remember very well an impression of a kind of internal dizziness , a sense of the inappropriate tension and speed in myself. I remember this feeling of being exposed…the juxtaposition of my own cultural situation against a whole cultural background of a different quality. It’s one thing to see this occasionally when you meet someone who has worked in this way for a long time, and has a relatively relaxed physical organism but to be in a society where this is part of the transmitted heritage witnessed in the physical bodies of people created a very strong impression of something that might be possible for people. That was an enduring impression.
RW: Earlier, you described some observations about their posture.
Seeba: It was very instructive to observe the people’s postures, standing and walking—where the line of the ear was in relation to the shoulder, and the position of the arm along the side of the body. People were moving from a more upright balanced position with the weight seemingly further down in the body. By contrast, in the West we see the hands are forward of the shoulder line(demonstrating) and the head, neck, and shoulder are projecting forward, sort of "into the future" if you will. Various compensations have to be made for this and one of the results is low back pain—which is the number one reason, I think, statistically, that people miss work nowadays. This projection into the future is very characteristic of our culture, where it’s always assumed that what’s most valuable, most interesting, always lies in the future, yet to be found. In the field of medicine and science it’s always the next discovery. This extreme emphasis on the future has repercussions on the form and function of the physical organism, and it can be seen in the posture.
RW: I realize I don’t have a sense of when exactly you pursued your medical studies in China.
Seeba: In 1979 and 1980. The course of study and practice was similar to the intern/ residency period in a Western medical setting, the final stages of medical school here. You actually begin practicing your medical techniques in a hospital setting under observation and supervision. We were some of the first Westerners permitted into China in the period just after the end of the Cultural Revolution. Their system of medical education was still reflective of the ancient master/student relationship. Even in the hospital setting there was this sense of personal relationship with the doctor/professors. You would do rounds and the like but there was much emphasis on the transmission of the seifu ‘s, or master’s, personal experience—insights gained as a result of the seifu’s personal being as well as the depth of his medical knowledge.
RW: You got some sort of degree then, through a Chinese institution, did you not?
Seeba: Yes, both from China and the U.S. When I started in Oriental medicine there was just beginning to be a level of standardization in education and licensing. One of the things the Communists tried to do was to gather all the knowledge that was held in family lineages and religious traditions. There was a lot of that. They tried to bring all this together and make it transmittable to the masses through institutions more or less the same way we do in Western medicine. Some people say that’s one of their contributions. Others would say it’s one of their failings, because of the breaking down of that master-student system.
RW: In the master-student system, you had to be able to reproduce his or her experience?
Seeba: It was more that way. You still had to know all the academic groundwork, the theory. You had to know how to build formulas, know the nature of herbs and how they were used, where acupuncture points were, meridian theory, symptom-sign complex differential diagnosis. But all that seemed to be considered a background to this other thing, the relationship with your seifu, which was considered equally, or even more, important. This system still existed somewhat in the U. S. when I studied here. I apprenticed with Doctor Yat Ki Lai who was part of a long lineage of traditional doctors. He would point out the uses of certain herbs and formulas which couldn’t be found in any text. These were his family’s secrets being passed on, part of his father’s and grandfather’s medical heritage. And so that aspect stood out in relief against a more traditional academic medical education.
RW: Is the practice of medicine more an art, or a science? Or, maybe you’d reflect on both of those aspects…
Seeba: Well, it’s a little difficult to speak about that without a conversation on what you might consider art to be. But if an "art of medical practice" alludes to an inner aspect—a less quantitative aspect that one tries to be a vehicle for—then in a modern medical/scientific education you might have a difficult time finding a correspondence. On the other hand, in actual clinical practice, in your personal relationship with the patient, there is over and over the sense that this other aspect is at the very heart of the healing process. And this is the most difficult part of medical practice. There’s a reason it’s called medical practice…and, you’re called the patient. Patience! It’s very tempting to fall back upon medical knowledge and technique as a way of avoiding the demands of this contact with the person before you, a contact that puts you in the presence of the hidden forces which both constitute and decompose us. An interest in this confrontation, and the effort to allow it, could be seen as the beginning of a "art of practice." Keep in mind that this is without diminishing in any way the necessity for the rigor imposed by medical science.
RW: Could you say more about this inner aspect one might be the vehicle for?
Seeba: Can I allow myself to be faced with the person, and not just his disease? This is a different demand, and the response to this begins to initiate a process which is a kind of artistic endeavor, if that’s not too strong a statement. The compelling force behind allopathic, or Western, medicine is to separate things, to separate the parts of the organism from each other. And there is a usefulness in this approach. But, in actual fact, this liver, diseased as it might be, is inside a person who has a history, a family, an emotional life, relationships and the like. And the real challenge, the "art" of medicine, is the attempt to relate to this whole without losing the discipline of the scientific requirements. Or, at the very least, to allow this attempt to have a life of its own, and to be included in the investigation of illness and healing. To try, both for yourself and in relationship to the patient, to come to an understanding that this process happening in me is not separate from all these other aspects of my life. To put it into an actual practice in a medical setting is doubly difficult, but without it, I think there’s not much hope for a medical system that will be anything more than a system of crisis interventions. "When you’re almost dead, I can keep you alive."
But keeping you from getting "almost dead" is the big difficulty in medicine—dealing with what it means to stay healthy rather than having to intervene when there’s a crisis at the level of tissue and organ. You have cancer which can be seen at a level of about a billion cells. Well, goodness sakes! By the time you can radiologically see something, it’s a billion cells, and what’s happened in between? We don’t relate much to that in our Western, allopathic traditions. Only in the last decade or so are we trying to have some relationship to that.
RW: There is a greater demand among patients to be received as a person. The only association I have about that for Western medicine is contained in that phrase, "a good bedside manner." But I gather that this aspect has more or less gotten lost in the technology.
Seeba: Yes. It’s built into the system that these aspects be de-emphasized. The intent and inclination among most doctors might be in this direction but it isn’t supported. I think there are probably many physicians who have left the profession out of frustration because of that. The system itself makes it very difficult to spend time with the patient, to take into account much more than the results of your lab tests. When you get caught up in a system like that it is very, very difficult to do anything other than what the system demands of you. And so, the doctors face more or less the same challenge as the patients do of how to carve out a more human relationship in the midst of these rather inhuman conditions. It goes along with the problem of trying to find ordinarily good food and ordinarily clean water, and conditions of life which can support a healthy organism.
RW: Could you say a little more about what you mean by "ordinarily good food" and "ordinarily clean water"?
Seeba: In the clinic one of the first things we do is talk to people about their diet. We ask them to try to eat foods that are organically grown, and people either burst into tears, or they go into attack mode. Right away you know you’re on to something. It’s almost an act of heroism, speaking from a clinical point of view, to get people to lead "an ordinary" life. What I mean is there was a time when you wouldn’t give a thought to something like drinking water from your well, or a spring. Foods were grown locally and there was never any question about it. You just ate them. And now, just to simply have water that’s pure, and air —you can only do so much about that—and foods that are uncontaminated is almost impossible for people. First to find them, and then to afford to do that.
RW: So, along with this, one of the important things for you is to be able to have "ordinarily human relationships" with your patients.
Seeba: Well, the other is certainly not very interesting and, in my experience, it doesn’t get very good results. So, if you want something more than just— if you have a leaky nose, I stop the leak, or a headache, I can temporarily obliterate the pain. That’s one level that can be sort of satisfying, except when you show up again in a couple of months and you’ve got chronic sinusitis now. That’s not very satisfying in the long term. But there isn’t much pressure to practice that way because—let’s come at it from another point of view: in a community situation where people are more or less stable, not moving around, and payment for my services comes directly from my patients and not from a pool of money separated from my practice—as with insurance—then there are certain legitimate pressures on me to relate not just to your headache but to what might be behind all that, to your life situation. My family knows your family. We live next door. I grew up in the same town. Everyone knows my shortcomings, and one thing and another, and so there’s a certain healthy pressure on me to relate to you. Whereas if I live in a big city and never have to worry about my patient load and I’m always going to be paid for my services—not by you, but from a pool of money that exists outside of our relationship—the situation is completely different. It’s very easy to let myself off the hook, and as long as I’m practicing within certain guidelines I’m protected from liability. So it creates a very strange situation from a human point of view.
RW: You’re endeavoring to practice in that old-fashioned way. The way you described that was community based.
Seeba: Attempting to practice medicine outside of the dominant medical culture in some ways gives one an advantage in that your time is more your own. You have to work a little bit harder and you certainly don’t make the kind of money you would if you were in that system. On the other hand it’s more interesting and, in the long run, I think we’re doing a better service for our people. Take the direct relationship with money, for instance. A fee for service puts you directly in relationship to the person. You know, this whole question of money is very embarrassing to all of us. There’s a tremendous amount of tension related to money. If you have a person paying you out of his own pocket, that creates a pretty interesting and demanding situation— both on the patient and on the care provider.
RW: I was struck by your handling of the money situation when I came to see you. You mentioned it ahead of time and basically put me very much at ease. I’d never had that experience with a care-provider before.
Seeba: If any aspect of your practice creates a condition which is going to jeopardize a possible favorable outcome it demands attention, and surely the money situation can create a great deal of unnecessary tension. It can be dealt with many ways—sometimes all that’s needed is a simple conversation, or setting up a payment schedule, or deferring payment, doing exchanges, or whatever is necessary from a practical point of view. But the money question has to be addressed. if not, it can lead to unnecessary difficulties between the doctor and patient. And I think it’s incumbent on doctors who work outside the reimbursement system of insurance companies, managed health care and so on, to try and find a way to make their practice available. Otherwise, what’s the point?
RW: At the same time, you need to make a living.
Seeba: There have always been plenty of patients coming through the door. It’s just been my experience that if the doctor makes this effort the other situation most often takes care of itself. There have been many interesting relationships around this issue. For instance, not too long ago there was a Native American woman whose tribe held rights to gather wild rice in Northern California and this was used as an exchange. Well, this was wonderful! It’s so expensive we don’t use it much in our household. Several patients keep the research files up to date, and so on. And so you end up building relationships with patients which makes it possible for them to get medical help, and you get the help you need. I just find that eminently practical, and interesting. And most often, the outcome, clinically, is more satisfactory.
RW: It’s a good example of how opening up an area creatively can really lead to another kind of richness.
Seeba: Well, surely, if the whole thing is economics, if the only reason a person is in the medical profession is just to make money, that can be done, but it’s hard to imagine that it would ultimately be very interesting. But still, you see that.
RW: I’d like to get your response to something Milton Erickson said. Do you know of him? I think it’s very interesting.
Seeba: I have a lot of psychotherapists in my practice and his name comes up a lot. I’ve got a couple of books by him.
RW: He said, "Never be impolite to the unconscious." Somehow I think of this applying to you, that it would fit your style.
Seeba: One of the things you see verified again and again in practice, and which is commonplace in the Oriental understanding, is that disease and the disease process originates in, or has an intimate relationship with, what we would call the less conscious, or unconscious, part. For instance, in Oriental medicine where historically there was practically no dissection for religious reasons they built up a whole series of observations called the poetry of ten questions. It was built up literally over thousands of years and was based upon countless observations of subtle inclinations, moods, tones of voice, patterns of breathing, and the like, all emanating from what we might call the unconscious part. And all this was noted in relation to disease process.
We’re beginning to get a hint of this in our Western research. For instance, in Oriental medicine the emotion of joy is related to the heart—not enough, too much, you end up with a heart problem. I remember seeing a survey of male coronary artery transplant patients, and to a man they expressed, in one way or another, a lack of joie-de-vivre. The underlying characteristic for all of them was that they’d lost heart. Another interesting statistic related to this is that most heart attacks, world-wide, regardless of culture, happen on a specific day, Monday, at around nine a.m. That’s when you’re starting your work week. You could say it means you don’t have your heart in what you’re doing.
Well, this is Chinese medicine. Each of the organ systems is associated—the liver with anger, the stomach with worry, the kidney with fear—each one has, you could say, its unconscious expression. In Oriental medicine feeling the pulse, listening to the person, how they express themselves, the color of their skin, what kinds of foods they like, could lead you back to the subconscious because these physical expressions would be related to these underlying parts. And so you have a two-way street. And why not? Really, how could it not be so that there wouldn’t be some bio chemical reflection of a dysfunction in the non-physical parts of the organism? It’s just difficult to quantify it. In my Western medical education, if I can’t quantify it, it makes it a little uncomfortable to speak about it.
RW: And yet this would be a very key element in your practice.
Seeba: Without that I couldn’t begin to practice. It’s very interesting because in Oriental medicine, once you get good at this type of medical observation, and you don’t have to have your pencil and paper in front of you jotting all these things down, you have conversations with people and at the end often you can make a very accurate diagnosis. They say, "where did you get all this information?" For the person who can see it, the information is there. It’s really fascinating.
RW: And your sensitivity to all those subtle things has become more educated, would you say?
Seeba: It’s a question of practice. But first there has to be a system. Someone had to collect the information and it had to be transmitted. In Oriental medicine we’re very fortunate to have a, more or less, intact system that’s survived and come down to us. It reaches back before recorded history. That is unique on the planet, I think. There are a number of ancient traditions of which parts have been preserved and aspects of shamanistic traditions which still do exist but nothing on the scale of Oriental medicine. So we’re fortunate, I think, to have access to a body of knowledge like that. And if one applies oneself in clinical practice to using that system one acquires a certain facility, as one would with anything one worked at.
RW: How many years have you been at this now?
Seeba: Let’s see, almost fifteen years when you include the time spent roaming around Africa in the early 1960s.
RW: I’ll have to ask you about Africa some other time because I’d like to know what—over this period of time, and making your own observations—what you can say you really know to be true—if you know what I mean.
Seeba: I would say the observation—the fact—that in the maintenance of health the most difficult issues are the most simple, most fundamental, and least emphasized. That is, the degradation of the food chain, our water, and our air, and conditions of our general social life. It’s absolutely the easiest thing in the world to leave out, the most difficult to address. Without addressing that in the vast majority of clinical situations, at best, your results are going to be limited, I think. I’m not speaking of crisis situations, but of general health and long term results. That I’ve verified for myself over and over again. Whether it’s arthritis, or chronic sinusitis, digestive problems, tumor formation, auto-immune illnesses, chronic fatigue, whatever it is, sooner or later you’ve got to back and look at what people are eating, how they’re eating, the type of water they’re drinking, and how they’re living. This is absolutely central. The way out of these problems are varied, and this is where the practice of medicine gets very interesting because there are a lot of different ways up the mountain. But without addressing these things the fundamental health problems are not getting addressed, in my opinion. These are probably the most important factors in the now epidemic degeneration of the health of our people in the industrialized world.
RW: I think this is the subject that really caught my attention when we first talked in your office.
Seeba: You can come at it from many different angles. For instance, simply take seed selection in industrial agriculture. For decades there’s been intentional selection of seed relative to shelf life. In industrial agriculture you need to have time to move large amounts of food from one place to another. Well, some of the very things that cause food to rot early are its enzymes that support good nutrition, if you will. So, if you get a tomato not to rot it means you have deprived it of the very enzymes the body needs.
This "de-enzyming" of the food has now been implicated in a whole range of clinical pictures. There are many other dramatic examples relating to this problem. There are certain molecules in our foods which come from petro-chemical derivative substances—herbicides, pesticides, and chlorine products—that contain a phenolated "a" ring which is identical to the phenolated "a" ring in the estrogen molecule. These lipid soluble toxins have an affinity for endocrine tissues.
There is a lot of evidence in the last few years that the now nearly epidemic increase of breast cancer and prostrate cancer, among others, is tied to the vectoring of this molecule through the food chain. It’s called hyper-estrogenation, and this all goes back to the industrialization of our food chain. Because it’s impossible to grow food the way we do without the introduction of massive amounts of chemical fertilizers, pesticides, and herbicides.
So you keep going back to the very basics of life which is the food you eat. All biochemical processes are tied to the food, and the air, and the water you drink. Common sense would have you go back to that. But it’s not taken with the kind of seriousness in the medical profession it should be, not even approaching what it should be. And frankly, there’s not a lot of money to be made from a type of medicine where you have to use substances that are non-patentable, for instance. So there’s no interest in trying to relate to this natural process involving the food and the air and how to deal with illnesses with therapies that are ecologically related to our own place in evolution, therapies that make use of botanicals naturally existing which have similar effects to those of analog medicines— because there’s no money in it. You can’t patent them and so there’s no impetus to use them.
Progesterone is a very good example. Progesterone is a product that many cultures, when you examine them, have used. For instance, among the Triaband people there isn’t even a word for menopause. There’s no concept of this passage, no breast cancer, endometriosis, ovarian tumors, etc. Of course, they have other health problems. But what we see is that on a daily basis they are eat a plant, the diascoria plant, which is where progesterone comes from. All progesterones have always come from the wild yam plant, but in order to sell it as a non-botanical, which means you can patent it, the molecule gets changed a little bit. It’s crazy. You have a molecule that’s more or less identical to the body’s naturally occuring one, and for economic reasons you change it a little and get "progestogen" which is given to women and has all kinds of side effects. You see that over and over again—the controversy between botanical, or planttract medicines and "artificial" or "man-made" medicines.
It comes back to this lack of appreciation of the very basics of health which goes back to agriculture and our attitudes toward natural products vs. "man-made" products, and to our attempts to manipulate processes that have been on the planet for a long, long time, without taking into account what the effects of that might be. As a result we end up with the situation we have in the world today which by anyone’s account has to be described as an epidemic of degenerative illnesses in the industrialized world. It even has some biologists contemplating the extinction of our species because the environmental estrogens are ubiquitous now. There has been about a 40% decrease in the sperm count in men since the introduction of these products into our environment. Taking that out on a straight line projection and you can see what could happen.
RW: Another alarming thing is the appearance of new viruses that seem to be beyond medical science’s ability to handle them.
Seeba: And also, the common bacteriums.
RW: There’s big problem there too isn’t there? In the popular press there’s the prediction of the eminent end of the effectiveness of antibiotics.
Seeba: This problem is now openly discussed in the popular press. As an example, my latest copy of the FDA Reporter, the official lay organ of the FDA, has as its lead story, "The Rise of Antibiotic Resistant Organisms."" Enterococcus, for example. It’s contracted in hospitals more than anywhere else and has mutated beyond any of the antibiotic treatments. If you’re strong, you survive. The common pneumococcus has at least six strains which are resistant to all antibiotic treatment. Scientists do not expect this trend to be reversed. The very thought that you would take something like a bacterium with its capacity to reproduce—every twenty fours hours is something like 1500 years on our scale of time—the very thought that these wouldn’t have the capacity to mutate is kind of ridiculous—and yet that was the assumption, I suppose, that the antibiotics would just keep on working into the future on a straight line, that we would always have antibiotics with us. Well, here we are, just forty years later. It’s hardly a breath.
RW: Yesterday I was listening to a British scientist talking about some enzyme he was working on that would stunt growth processes so the stalks on wheat, for instance, would remain fairly short. They would be stronger and could withstand rain and wind storms better, and would be easier to harvest, I guess. This scientist was talking eloquently about the chemistry and it was all very impressive, and yet it kept reminding me of some Monty Python skit. I could just see this scientist in his laboratory working on these very intricate problems without a thought about what this meant in the bigger picture. And you have that multiplied thousands of times. Your description of what has happened with antibiotics and bacteria is a good example of this.
Seeba: It brings me back to a fundamental question. What is the place of this type of activity? Is there something missing in this approach? I think rather odd distortions occur when there are no underlying questions which can relate this type of functioning to the organism as a whole. The very fact that a certain molecule can be created that causes an effect in the organism is considered an achievement. But there’s not sufficient thought given to the consequences for the whole organism. Antibiotic therapies and the way they are used is a very good example of this. It brings me again to the consideration of what question, what approach could relate this part(which searches for answer to scientific questions, for instance) to something more whole—my own life, the life of the community, the community in relation to the whole planet.
RW: The story of The Sorcerer’s Apprentice just came to mind. It seems an appropriate metaphor.
Seeba: Yes. And I think one of the fundamental conditions related to this situation is reflected by what I hear frequently in our clinic. People often say, "I want to relax but I don’t know how. I’ve got a sense that part of my problem is connected with tension and stress." They express that in many, many ways, but it is connected to a recognition of a condition which exists as a consequence of something less visible or accessible . And commonly, with some discreet testing you find a state of exhaustion.
Well, what is behind this, and how does it begin? It’s very interesting. Here’s an infant looking out, there’s no expression, and you can sense the world is just being taken in. And then, what happens? Everyone gets this impulse to stimulate the child, to get it to react, to do something. By adulthood you’re considered a person of great enthusiasm and energy! You have two or three jobs and you’re running around hebephrenically. Isn’t that great!? And God help you if you get caught watching too many sunsets out at the beach! Someone soon wonders if you’re okay and suggests a psychiatrist you can talk to.
The Chinese say we in the West live in a very Yang environment where everything is push, push, action, do…with little reflection, little of the natural restraint which comes from a questioning attitude. And we see this reflected in people’s physical situation with these exhaustive states in the adrenal, thyroid, immune, and other regulatory systems. And you see, it begins at the very beginning.
RW: At the very beginning we’re conditioned to be in the state of stimulation.
Seeba: And to sit quietly is considered a cause for psychiatric concern. If you see a person who’s quiet the first thing you think is that they might have some kind of mental or emotional problem. On the other hand, if you’re running around doing four or five different things you’re congratulated. So what happens? What types of tensions must get set up unconsciously in the organism when this necessary food is missing, and its very pursuit is held in suspicion? Depression is a very good example of this problem. In former times depression used to be called melancholy. Care of the Soul by Thomas Moore has a very good chapter on this.
There was a time when what we call the state of depression wasn’t treated as a clinical symptom but as a bearer of a kind of knowledge, which only that state of melancholy could bring. There were even places in gardens set aside where one would go to sit with this state. There was a reverence for this state as a bearer of a unique type of knowledge—of my own mortality, for instance. One can find many examples in clinical practice where our entire education steers us away from the kind of "food" our organism is begging for. The very voices of the physical organism often come to be treated as pathological. If the symptoms get too strong—you appear hysterical in the doctor’s office—you’re given valium, or strong pain relievers.
RW: When I first talked with you, you said something like "Only when the body is dying in big enough numbers—no escape in the board-rooms or in the rich sections of town—then some of these problems may start to be addressed.
Seeba: More and more, it seems to me that the final battlefield, the final arena, in which these environmental and social problems are being, and will be, played out is in the human organism. No matter where you are, no matter what your social position is, no matter how much money you have, you will not be able to escape the effects. This is where, finally, perhaps one’s attention can be shocked enough, galvanized enough to look at the situation directly.
RW: It seems true.
Seeba: When I feel that my life is a stake, my physical life, I think there’s a possibility that doesn’t exist when I can just make an accounting sheet of whether there’s enough money to be made here, or I can just move over there. When it really comes down to the realization that my life, and human life, in general, is at stake, as horrifying as that is, a new possibility arises. I think this is what we are approaching very quickly, especially in our industrialized society where the effects of these types of imbalances are so obvious, so increasingly obvious—interestingly enough, in the reproductive system.
RW: Is that the most sensitive part of the organism?
Seeba: To certain of these molecules. They seem to have an affinity to testes in men. Testicular cancer, prostrate cancers are about the same ratio as breast cancer in women, around one in eight. It’s epidemic by anyone’s calculation. And the whole endocrine system, the pituitary, the thyroid, adrenals, the whole regulatory system—these tissues seem to be very sensitive to this influence also.
RW: I wonder if there’s a kind of direct analogy between the disorders of the body and the disorders of society? Perhaps so.
Seeba: Indeed. One of the chief complaints that I hear clinically, is fatigue. So, how do you address fatigue? If, in your whole world what’s of value is stimulation and activity, and you’ve got fatigue, my goodness sakes, what are you up against? You see the confrontation—between our world where activity is the value, and your own physical situation, which is lack of energy. You’ve got all these little short term solutions, sugar, coffee, alcohol, cigarettes, drugs that stimulate. Or, if the pain of it all is too much, there are the drugs that obliterate. It’s not a question of why I’m exhausted, but of finding strategies of getting enough energy to face the next day. And the very things being used to get to the next day eventually will cause a collapse somewhere.
* Cal Seeba passed away in Feb. 2021
About the Author
Richard Whittaker is the founding editor of works & conversations and West Coast editor of Parabola magazine.
SUBSCRIBE NOW
TO OUR MONTHLY NEWSLETTER









Share Your Comments and Reflections on this Conversation:
On Dec 23, 2021 Del wrote:
Seeba is way ahead of his time, and society is behind.On Aug 4, 2009 Jeff wrote:
Great learning in this conversation.Peace Out